What is the Difference Between a Coma and Brain Death?
Answer: A lot.
UPDATE: If you have family or loved ones currently in the hospital and you are discussing the potential to donate and save lives, click here.
Coma
Coma is a state of unarousable unresponsiveness.1 A coma is a deep state of eyes-closed unconsciousness where a person is not able to respond to people or the environment around them. In a coma, a patient is alive and there is some brain activity. Depending on the severity of the injury, recovery time varies and comas can be temporary or permanent.
Patients in a coma might have brain stem responses, spontaneous breathing and/or non-purposeful motor responses. Coma has three possible outcomes: progression to brain death, recovery of consciousness, or evolution to a state of chronically depressed consciousness, such as a vegetative state.
Patients in comas are not considered for organ, eye, or tissue donation.
Brain Death
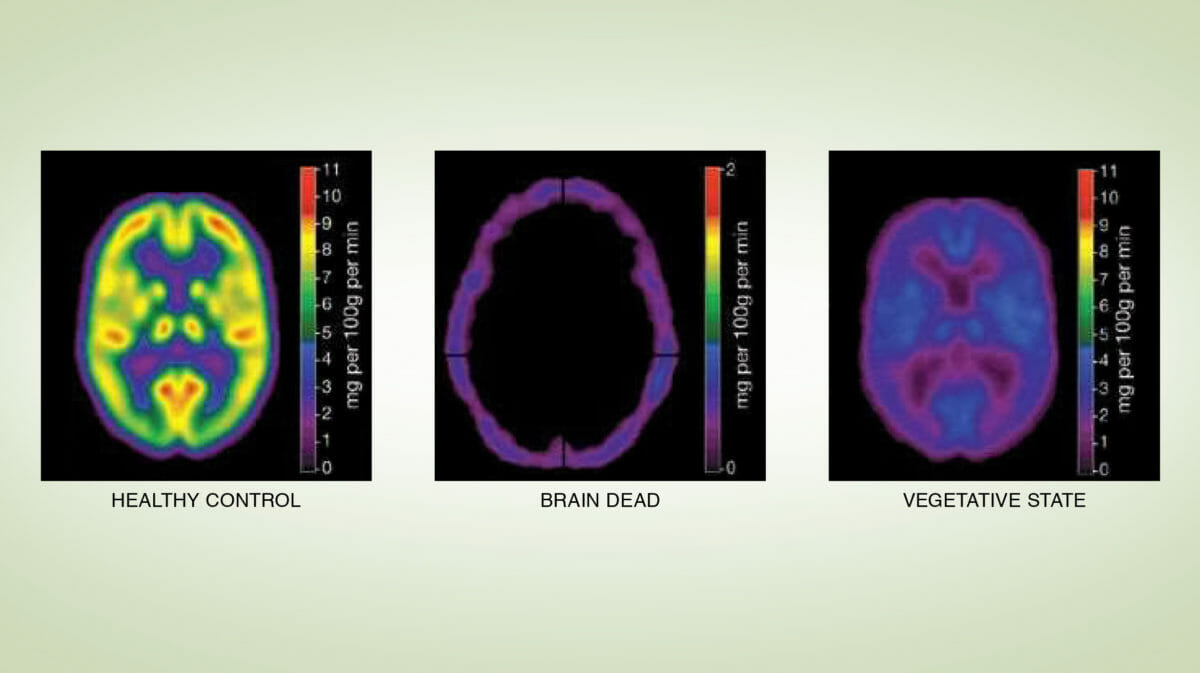
According to the American Academy of Neurology, “Death by neurologic criteria, commonly referred to as brain death, occurs in individuals who have sustained catastrophic brain injury, with no evidence of function of the brain as a whole, a state that must be permanent.”2 Brain death is legally and medically recognized as death. Brain death results from swelling in the brain; blood flow in the brain ceases and without blood to oxygenate the cells, the tissue dies.
The brain performs many functions, including thought, movement and all the neurological functions that allow the body to maintain blood pressure, heart rate, body temperature, hormones, breathing, etc. When a person deteriorates to brain death, the body’s entire system stops. You cannot breathe, your heart cannot beat and your body cannot function once your brain dies. Massive artificial medical measures must be started to maintain organ function (such as ventilated support), but these interventions are only a temporary measure.
Brain Death Testing
Organ Procurement Organizations (like LifeSource) do not make determinations of brain death. Instead, hospital clinicians who are separate from the donation and transplant process are responsible for determining and declaring death.
Physicians and health care providers conduct a comprehensive assessment to determine brain death, performing several tests to confirm there is no brain activity in accordance with strict medical standards.2
Only after brain death has been confirmed and the time of death noted, can organ donation become a possibility.
Donation After Brain Death
Families of a brain dead patient must, by federal regulations, be provided the option of organ donation. If the family declines donation, the mechanical ventilator, medications and fluids are discontinued, after which the heart stops. If the family says yes to donation, the regional organ procurement organization (LifeSource in MN, ND, SD) is involved. The donor’s body is kept functioning by artificial means, such as ventilated support until the recovery of organs and tissue for life-saving transplant.
If you support donation it is important to document your decision. This removes the burden off of your loved ones to make the decision once you have passed away.
Citations:
- Tindall SC. Level of Consciousness. In: Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd edition. Boston: Butterworths; 1990. Chapter 57. Available from: https://www.ncbi.nlm.nih.gov/books/NBK380/ ↩︎
- American Academy of Neurology. (2023). Pediatric and adult brain death/death by neurologic criteria consensus guideline. https://www.neurology.org/doi/10.1212/WNL.0000000000207740 ↩︎
Photo credit: Nature Reviews Steven LAUREYS MD PhD FEAN.
 Skip to main content
Skip to main content
